Originally published on 1Jul23, edited 9Aug25.
On 26Jun16 my father, Francis William “Bill” Boylan died from prostate cancer. He was 86 years old. It seemed fitting that “our” story be released on the day of his passing, but the unexpected death of his brother, my uncle John Boylan, led to a delay.
Uncle John was there for Dad when he needed him, taking him to his oncology appointments at The James Cancer Hospital, part of the OSU Medical Center. He drove Dad to his doctor’s appointments, some 50 miles away, for the duration of his treatment and was otherwise there when needed.This article is dedicated to their memory.
What is written below is based on my personal experience, research, observation, and conversations with my medical team and should not be construed as medical advice. It is intended to raise awareness and encourage others to be diligent toward monitoring their own prostate health. Links to various prostate cancer information resources follow this article.
Here goes . . .
This is my story. And my father’s story. It is also the story of countless millions of other men, past, present and future. While each patient’s story is unique to him, we all share commonalities. Family, friends and co-workers are affected. We have to consult multiple doctors and make tough decisions. We all suffer emotional and psychological effects. And we all need information to guide us toward the right treatment strategy for us.
The single-most important aspect of any treatment program is early detection.
 |
| absolutelyrealtruefacts.com |
in 6, or 16.67%. This also means that 13% of spouses will have a husband with prostate cancer. If a revolver had eight cylinders rather than six, would you be more willing to put the gun to your head and pull the trigger? Not me. No way. But that is what most guys are doing. We are unknowingly playing Russian Roulette by not seeking regular prostate health screening. (See Risk Factors)
My father was not one to talk about things. Anything. He never told me he had prostate cancer or that he would die from it. I had to learn these things from a sister who was helping care for our mother and later, Dad. Prostate cancer must be talked about. I had no idea that if one’s father had prostate cancer, his sons are more likely to have it. We must talk about it with our sons, our fathers, friends and family, regardless of gender.I first came to suspect I might have prostate cancer, (PC from here out), last August. While back east in July, my dear friend Beth pointed out that I had lost weight. She and the friends we were with made me promise to see a doctor. (My weight had dropped from 165 lbs. to 143 lbs., a loss of 13.33%.) My general practitioner ordered blood tests and on August 5th, they revealed a PSA (prostate specific antigen) level elevated to 5.8. I was referred to a urologist.
A normal PSA level is below 4, although it is possible to have PC with lower PSA levels and not to have it with higher levels. The surest way to determine if one has PC is to perform a biopsy, a procedure usually performed by a urologist. At the time, I did not have insurance, so put it off until Medicare kicked in. On 20Jan23, I was informed that I have prostate cancer.
Many are familiar with Clark Howard, a consumer advocate who had a radio program, (and now a podcast), that I listed to when living in Connecticut. He also has PC. In a short video posted on YouTube, he says, “If you get a diagnosis of cancer, you’re automatically going to freak out . . ., let’s call it like it is, full freak out mode.” Boy, is he right about that!
I freaked out. I didn’t know what to think, what to do. I don’t have a spouse to turn to. I didn’t want the guys I work with feeling sorry for me or treating me like some invalid. As it is, they look out for me because of my age, not wanting me to carry heavy materials and so forth. (How else are you supposed to keep in shape if you don’t do some heavy lifting?) They are a great group. We are like family, we take care of each other, bickering like siblings one minute, pals the next and when someone needs support, we’re there for him.
A couple of the guys knew and were sworn to secrecy. A couple weeks ago, when I came forward and told the rest of the crew, no one seemed surprised, so I suspect the cat had already been let out of the bag.
I had to turn somewhere in the family. I called Uncle John. After all, he was the family patriarch and was there for Dad. True to form, he was there for me, too, offering moral support and a listening ear.
I also turned to his son, my cousin Joel, who is a medical doctor. He was with me 100%. Like his father, he offered moral support and a listening ear. He also provided me with links to the National Cancer Institute and American Cancer Society. Joel offered good, common sense advise concerning overall health and advised me to do my own research and put together a list of questions to ask my doctors.
Joel helped launch a research project that led to over 50 sources of information on PC. (See bibliography) As a result, I went back to my doctors with sixteen pages of notes and questions. Joel and I continued to talk and share information. He told me that I probably knew more about PC than he did!
Uncle John and Joel were both sworn to secrecy. I did not want anyone to know I had prostate cancer. Their support and encouragement were immeasurable. Without them, I would not be where I am today. Regrettably, Uncle John passed away on the morning of Father’s Day, 2023. I was getting ready to go see him when I got the news from Joel’s brother, Jeff. It was totally out of the blue and unexpected. It hurt. Badly.
Uncle John, also a USAF veteran, was laid to rest with full military honors on Friday, the 23rd. After the funeral, the family gathered for a meal provided by the church, as is customary. When we prepared to part ways, it slowly came out that all the first cousins knew. And I’m glad they did. Their display of genuine caring and support was needed. It touched me.
Between the close-knit friends back east, the guys at work, now the family and more-local friends and neighbors, I have a strong support network. I guess that is why I’m getting so personal; to emphasize the importance of having support.
Back to full freak-out mode.
 |
| Dimitrious Stanley 1974 -2023 |
receiver, Dimitrius Stanley. He was also an every-Friday guest on a local radio program, The Mark Blazor Show, where he had been given the nickname, “The Guv’na”. He had prostate cancer and regularly spoke about it on the air. Back in October or November of last year, he suddenly stopped appearing, though he would on occasion call in. Knowing a couple of people who had undergone cancer treatment, I just assumed that the treatment had caught up with him and he would be back on the air, once he recovered. (After all, he was a young man.)
On February 9, 2023, 20 days after my diagnosis, Dimitrius Stanley passed away at 48 years of age. Diagnosed at 44, he fought the cancer for 4 years. When I heard the news, I cried for the first time since my own diagnosis. Dimitrius was a gentleman and a gentle man, a man who cared about his country, his state and his fellow Man. Though we never met, I still miss him. His life, his spirit and determination were an inspiration, not just to me but to many others.
I printed numerous copies of his picture, posting them around home and on the dashboard in the car, where I could look toward him when I needed strength. I found myself talking to him, frequently. To this day, I talk to him and almost believe he answers me. Maybe he does.
While doing a bit more research on “The Guv’na” for this article, I learned something that makes me think he really did hear and answer me . . .
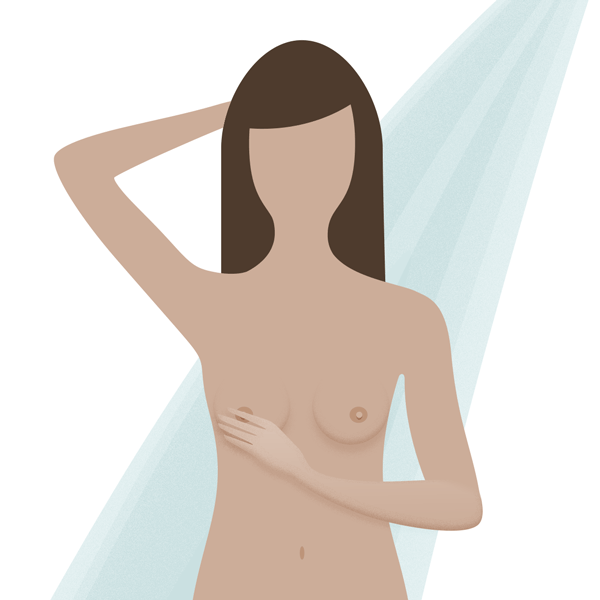 |
| National Breast Cancer Foundation |
After our conversation, I decided, “the heck with it”; it's time to come forward. Prostate cancer needs to be talked about. I have a platform from which to speak, along with a substantial social media circle through which to share, and a few broadcast and print media connections, in two states.
Back to “The Guv’na” . . .
. . . I learned he founded a non-profit to help men (and their families) pay for the tremendous costs of PC treatment. On the website, under “My Story” he writes the following, “My hope is to raise awareness through my foundation, Brave Men Inc, by gaining knowledge through our research and sharing this valuable information with the public. Prevention is key so let’s work together to end this terrible disease that is ravaging men’s bodies all around the world.”
Could it be Dimitrious actually heard me in my freak out and guided me toward coming forward? Could be. Our goals are virtually identical; to raise prostate cancer awareness and to share the benefit of our experience with others in order to help them.
Back to my story . . .
A few weeks ago, a course of treatment was decided upon. I was anxious to get started but there was a delay in getting a certain medication. Anxiety is common in cancer patients.
A week prior to Father’s Day, all that occurred over the last five months came to a head and I just could not go on. I had to have a break, my work performance the Thursday and Friday before, falling off dramatically. It would not be fair to my co-workers or my employer to go to work in such condition. I took a week off. The short sabbatical performed wonders. It allowed me to decompress and get my home in order; carpet and furniture cleaned, office work organized and filed, some gardening done. All at an easy pace, no pressure. I rested.
Then Uncle Johnny died. For the second time since the cancer diagnosis, I cried. As hard as that was to deal with, without the time off it would have been impossible to come to Jeff and Joel’s support, small though that was. Funny, isn’t it, how the timing of events beyond our control works out?
Back to January and the road to selecting a plan of action.
A prostate biopsy showed cancer prevalent on the entire right side and mildly present in one area on the left. In six areas, the Gleason scores were three at (3+4=7) and considered to have a good outlook, three at (4+3=7) which is more aggressive and likely to spread, and one (3+3=6), a low risk. Based on that, I had Stage II cancer. Once my urologist had those results, he ordered a PET Scan.
Twenty minutes prior to the scan, the Tech injected me with a radioactive tracer. Once on the machine, the table moved back and forth in the chamber while the scanner spun around me. Kind of boring, nothing at all like a Cedar Point rollercoaster ride.
The scan revealed the cancer had spread into the right seminal vesicle, raising the staging from Stage II to Stage IIIB. The seminal vesicles are small glands located between the bladder and rectum.
This involves removing the entire prostate, including the seminal vesicles. I’ll not get into the risks or side effects, here. (More info in the appendix.) Let it suffice to say, I did not like them. We discussed the questions I’d prepared. Every other form of treatment I asked about was rejected.
I told the doctor it was out of the question and asked for referrals for second opinions. He referred me to another urologist, (which I passed on knowing I’d get the same recommendation), then to medical and radiation oncology.
I saw the medical oncologist, first. Of course, he had a different recommendation. We too discussed my questions, and all other forms of treatment were rejected. His recommendation was hormone therapy, (androgen depravation), for 18-36 months. The one-word sentence he used sent chills through my body, “Castration”.
The first question for my doctors was, "how long I would live if I decided to forgo treatment"? He told me one to two years. He also said this had been going on for only five “or more years”. I began to mentally prepare myself to die. (What do I do with all those topographic maps and nautical charts?) The freak out skyrocketed.
Androgen depravation therapy (ADT) shuts down testosterone production, (see appendix) effectively rendering a man impotent and without interest is sex. It can take two years for testosterone levels to recover to normal, if they recover. The testicles become so small they cannot be detected. Other side effects include osteoporosis, decreased mental sharpness, increased risk of dementia and loss of strength. These things alone could put me out of work, permanently.
I will not be castrated, chemically or surgically. I will not live like that. It is not living; it is a mere existence! Three years of treatment, followed by two years of recovery make the process five years long! I would be over 70 years old by then. There is no guarantee of full recovery. No woman is interested in a man who is impotent. How could any man, in good conscience make such a recommendation to another man? He’s off the team.
Then, Nurse Practitioner Kelly Slavens called. We spoke for nearly 40 minutes. She is a gem. I asked her many of the same question I’d asked the doctors. She thought I could live another ten years without treatment and thought the PC had been going on for likely ten years. That means my father and I had PC at the same time. "Like father, like son". It also coincides with a diagnosis of having a "slightly enlarged" prostate. I didn't understand the implications, it was not explained to me, and it was not followed up on. Be forearmed; ask educated questions and follow up.
Kelly’s talk helped lift the dark cloud that had consumed me. I wasn’t going to die. I would recover, whole and intact. She told me about a new FDA approved drug, Orgovyx. While it too, is a form of hormone therapy, it is only used for 6 months, and testosterone levels return to normal in about two months. Kelly said the Orgovyx treatment would be used in conjunction with radiation.
In my research notes, I’d written that hormone therapy is not for me, unless as a short-term complementary treatment. Prophetic insight? Pre-destined?
Life teaches many lessons. One such lesson, often hard learned, is to trust your instinct. After talking to Kelly, I had a really good feeling about the treatment plan we discussed. My gut instinct pulled toward it. Though, like President Ronald Reagan said; “Trust but verify”. I did. Due diligence affirmed what we discussed. It verified that the long-term risks are minimal, potential side effects are minimal or easily tolerable, the recovery time, quick.
Next stop, radiation oncology. A meeting with Dr. Wang further served to raise confidence in this treatment combination. Like with the other doctors, only in greater detail, we discussed my questions. The conversation was informative and productive.
My gut instinct was affirmed. This is the right way to go. I accepted the treatment plan and Dr. Wang said he would set the wheels in motion.
There was one further obstacle to overcome, though. Orgovyx, being a new-to-the-market drug, is expensive. Without insurance, the drug costs $16,000 – $17,000 for a six-month supply. With my Medicare plan, the out-of-pocket cost is $5,400. I was prepared to pay it. How do you put a price on your health and quality of life? As it turned out, the Orgovyx manufacturer offers financial assistance. I didn’t think I’d qualify for it, but I did. (I never thought about financial aid. It’s out there, if you need it. Seek and you will find. Start with bravemeninc.com.)
While the Orgovyx arrived on the 21st, because of the potential for certain side effects, I delayed starting the medication until the evening of June 23rd, the day Uncle John was laid to rest. That was also the last day I smoked a cigarette. Certainly, there is something symbolic, there. (To date, there have been no side effects from the Orgovyx.)
The radiation treatment, in order to be more accurate and to prevent damage to surrounding tissues, requires gold markers be placed into the prostate, where they will remain. These markers provide a very narrow target for the radiation device to focus on. Also, a spacer is placed between the rectum and prostate, further reducing the risk of collateral damage. This will be done in late July.
Following that, I’ll be fitted with, for lack of a better word, a "seat" conforming to my body. The purpose is to keep the body in a precise position to assure consistent accuracy of the radiation treatment. At the same time, a CT simulation will be performed, which serves to locate and focus on the area to be treated.
External Beam Radiation. (There are internal forms of radiation.) There will be 28 treatment sessions, 5 days per week ending around the first of October. The treatments last just a few minutes each; in and out the door in 20 minutes. The James Cancer Hospital offers treatment up to 7:00 PM, it will not be necessary to miss much more work.
After treatment, begins active surveillance, which likely will continue for the rest of my life. At first, if I recall correctly, I’ll be examined (for PSA levels), every six months, then annually thereafter.
The prognosis is good. I’m highly confident in the treatment program I chose and in my care team. Today, I’m at ease. It’s all come together, nicely. The treatment has started and the “strategery” to complete it is laid out. A lot of people have prayed for me. If I’m gonna believe Dimitrious has reached out to me, I gotta believe that those prayers have helped, too. There is definitely a mental, psychological, and certainly a spiritual link to a positive outcome, and I don’t doubt I’ll come out of this in good health and good spirits.
In summary
All men are at risk of developing prostate cancer; no family history required. Early detection is key, (the average age is 66). It saves lives. It makes for shorter, less invasive or radical courses of treatment, with fewer risks and fewer long-term consequences.
While sources recommend starting at later ages, my personal belief is that if you are a Black man, start having your PSA level tested at age 30. Test every three years and at age 40, test every year. Non-black men, start at age 40. Test every three years and at age 50, every two years. At age 60, start testing every year. A PSA test can be conducted as part of a regular physical checkup which should only cost a couple hundred bucks, if you are not insured. Well worth the investment.
If you are diagnosed with cancer, go ahead and freak out. It’s normal. Just don’t let it consume you or keep you from fighting back.
Most of all, communicate. Talk to your children, parents, spouses, especially if there is a family history of cancer. (See Risk Factors) Make sure they are equipped with knowledge ahead of time so they can be pro-active.
Following are some details concerning risk factors, symptoms, complementary treatment options and various medical treatment options:
Risk Factors
For unknown reasons, Black men have a greater risk of having PC and it is more likely to be aggressive or advanced. Remember Dimitrious Stanley.
Prostate cancer feeds on testosterone. Body builders with prostate cancer who are given testosterone or drugs to increase testosterone production, will have a more aggressive and faster growing cancer. I know of someone in this position. He is only 53 yrs. old and his cancer is advanced. His sister had breast cancer.
In the early stages of PC, there are often no outward symptoms though a digital exam can detect an enlarged prostate. Later, more advanced stage symptoms include trouble urinating, decreased force in the stream of urine, blood in the urine, blood in the semen, bone pain, erectile dysfunction and losing weight without trying.
Complementary Treatments
Complementary methods can include vitamins, herbs, and special diets, or other methods such as acupuncture or massage, to name a few. Turmeric is one such recommended supplement.
Medical mushrooms have been used for centuries to treat infections. For several decades, mushrooms have been approved as a complementary cancer treatment in China and Japan. NuCana, a Britain based pharma company, is developing a mushroom-based cancer treatment derived from mushrooms found in Eastern Europe. Clinical trials are underway and should be complete in just a few years.
Prostatectomy is the removal of part of the prostate. Radical Prostatectomy is removal of the entire prostate. There are various surgical techniques used for prostatectomy. They include:
Radiation uses high-energy rays (like x-rays) to kill cancer cells. It can be aimed at the prostate gland from a machine outside the body. Or in some cases, small radioactive pellets, or seeds, each about the size of a grain of rice, can be put right into your prostate.
Current methods such as conformal radiation therapy (CRT), intensity modulated radiation therapy (IMRT), and proton beam radiation help doctors avoid giving radiation to normal tissues as much as possible. These methods are expected to increase the effectiveness of radiation therapy while reducing the side effects.
Common side effects of radiation to the prostate are diarrhea, leaking stool, or blood in the stool; having to urinate a lot, leaking urine, burning when you pee, or blood in your urine; erection problems, feeling very tired (fatigue); and fluid build-up in your legs.
Brachytherapy/MARS
The most appealing of all the various option was this. Unfortunately, because of the stage of the cancer, my doctors ruled this out.
Along with monoclonal antibodies/small molecule drugs . . .,
Brachy delivers radiation with a small radioactive pellet that is about the size of a grain of rice. The pellet (or pellets) are positioned precisely inside the patient’s body, close to or inside the tumor. In some cases, the pellets remain in place for just a few minutes. Other times, they are left in place for several months.
Brachytherapy allows doctors to deliver radiation directly to the patient’s tumor while limiting radiation exposure to healthy tissue.
MRI-assisted radiosurgery (MARS), refers to the method of implanting the radiation seeds. It allows for more precise delivery of the radiation with fewer side effects.
Side effects from MARS are minimal. Most patients return to normal activities the day after the procedure. After treatment, patients can return to normal sexual activity. Incontinence is rare, but some patients may experience temporary urinary side effects. These include burning, frequent or urgent need to urinate. These side effects can be managed with medication and typically resolve a few months after treatment.
Hormone Therapy
Several newer forms of hormone therapy have been developed in recent years. Some of these may be helpful when standard forms of hormone therapy (chemical castration) are no longer working. Some examples include abiraterone (Zytiga), enzalutamide (Xtandi), and apalutamide (Erleada), which are described in Hormone Therapy for Prostate Cancer. Others are now being studied as well.
Hormone therapy alone does not cure prostate cancer.
Hormone therapy may be used, (as in my case), along with radiation therapy as the initial treatment, if you are at higher risk of the cancer coming back after treatment (based on a high Gleason score, high PSA level, and/or growth of the cancer outside the prostate). Prostate cancer feeds on testosterone. Hormone therapy can be used before radiation to try to shrink the cancer (by starving it) to make the treatment more effective.
Possible side effects from long-term treatment
Orchiectomy (actual castration) and LHRH agonists and antagonists can all cause similar side effects from the lower levels of hormones such as testosterone. These side effects can include:
Reduced or absent sexual desire, erectile dysfunction (impotence), shrinkage of testicles and penis, hot flashes, breast tenderness and growth of breast tissue (gynecomastia), osteoporosis (bone thinning), anemia (low red blood cell counts), decreased mental sharpness, loss of muscle mass, weight gain, fatigue, increased cholesterol levels and depression.
Chemotherapy - Chemo
Chemo is the use of (non-hormonal) drugs to fight cancer. The drugs may be given into a vein or taken as pills. These drugs go into the blood and spread throughout the body. Chemo is given in cycles or rounds. Chemo may be used if the cancer has spread outside the prostate gland. It’s not used for early prostate cancer. Studies in recent years have shown that many chemotherapy drugs can affect prostate cancer. Some have been shown to help men live longer. Chemo is also used to relieve symptoms associated with advanced or metastatic disease, to improve surgical outcomes and in conjunction with hormone therapy, also to improve outcomes. It can also prolong the lives of patients who are no longer responding to hormone therapy.
Other new chemo drugs and combinations of drugs are currently being studied. (There are 38 or so different drugs used to treat prostate cancer.)
Side Effects of Chemo
Chemo can make you feel very tired, sick to your stomach, and cause your hair to fall out. These problems go away after chemo treatment ends. It can also cause mouth sores, loss of appetite, diarrhea, increase the risk of infection due to reduced white blood cells, easy bruising or bleeding due to reduced blood platelets.
These are some of the more common treatments for prostate cancer.
Other treatments include vaccines that treat, rather than prevent PC, targeted therapy drugs that target specific parts of cancer cells, altering the way a cancer cell grows, divides, repairs itself, or interacts with other cells, and immunotherapy which uses substances made by the body or in a lab to boost, direct, or restore the body’s natural defenses against cancer. Other treatments are being explored and tested.
In no particular order:
Chas Averbook: Prostate Brachytherapy Patient Story | Cleveland Clinic
Prostate cancer survivor: I’m grateful for treatment at MD Anderson | MD Anderson Cancer Center
Homepage | ORGOVYX® (relugolix) | Patient Website (Info on financial assistance is under the support tab.)
Orgovyx: Side Effects, Cost, Use for Prostate Cancer, and More (healthline.com)
Orgovyx: Uses, Dosage, Side Effects, Warnings - Drugs.com
Orgovyx: Uses, Side Effects, Interactions, Pictures, Warnings & Dosing - WebMD
How Cancer Can Affect Erections | Adult Males with Cancer
Complications of laparoscopic radical prostatectomy–A single institute experience - ScienceDirect
Targeted Therapy for Cancer - NCI
Support Services Locator - National Cancer Institute
Radiation Therapy for Cancer - NCI
Microbiome-Friendly Foods | Prostate Cancer Foundation (pcf.org)
PCF-Curing Together | PCF | Prostate Cancer Foundation | Prostate Cancer Symptoms
Perineural Invasion in Prostate Cancer: What It Means for You (healthline.com)
Survival Rates for Prostate Cancer
Prostate Cancer Stages | Staging of Prostate Cancer
Hormone Therapy for Prostate Cancer (ADT) | Prostate Cancer Foundation (pcf.org)
Hormone Therapy for Prostate Cancer
Hormone Therapy for Prostate Cancer Fact Sheet - NCI
Understanding Side Effects of Androgen Deprivation Therapy - CancerConnect
External beam radiation for prostate cancer - Mayo Clinic
Proton Therapy for Prostate Cancer | Johns Hopkins Medicine
How mRNA Vaccines Might Help Treat Cancer - NCI
Side Effects of Radiation for Prostate Cancer Vs. Benefits (healthline.com)
Possible Side Effects of Radiation Treatment for Prostate Cancer | OncoLink
Cancer Treatment Vaccines - Immunotherapy - NCI
What’s New in Prostate Cancer Research?
Prostate Cancer Treatment - NCI
NCI Search Results - NCI (cancer.gov)
Complementary and Alternative Medicine (CAM) - NCI (cancer.gov)
NCI Search Results - NCI (cancer.gov)
PDQ® Integrative Therapies Summaries - NCI (cancer.gov)
12 Questions to Ask the Medical Oncologist (webmdhealth.com)
male reproductive system diagram at DuckDuckGo
Radical Prostatectomy | Johns Hopkins Medicine
Surgery for Prostate Cancer | Prostatectomy
Search Cleveland Clinic | Cleveland Clinic
Radionuclide therapy, how it works | IAEA
Targeted Radionuclide Therapy: A Historical and Personal Review - PubMed (nih.gov)
targeted radionuclide therapy at DuckDuckGo
Radiation Therapy for Cancer - NCI
definitive radiation therapy for prostate cancer at DuckDuckGo
FDA Approves Relugolix for Advanced Prostate Cancer - NCI
Complications of laparoscopic radical prostatectomy–A single institute experience - ScienceDirect





No comments:
Post a Comment
The South Central Bulldog reserves the right to reject any comment for any reason, without explanation.